-
Effective January 1, 2020, adult Medi-Cal eyeglasses benefits are restored for eligible beneficiaries
ages 21 and older. Counties of San Luis Obispo, San Mateo, and Santa Barbara will be joining the rest
of the State and will now use CALPIA labs to fabricate Medi-Cal lenses. Providers will bill dispensing
services to the Medi-Cal managed care plan or to Medi-Cal as a straight/fee-for-service.
-
The PIA lab accepts jobs for both fee-for-service (straight) Medi-Cal and managed care Medi-Cal
beneficiaries. What are the requirements for getting a PIA account?
PIA account requirements are:
-
Applicant must be enrolled as a Medi-Cal Fee-for-Service provider with the Department
of Health Care Services or as a Medi-Cal managed care plan provider.
For applicants who are only managed care providers, you must also be enrolled as
an Ordering/Referring/Prescribing (ORP) provider.
-
Business address must match the professional licensing board records.
-
Business Address must match Medi-Cal and/or Medi-Cal managed care vision plan provider
records (i.e., Medi-Cal Provider Enrollment, Vision Service Plan).
The “business address” must be a physical location where services, goods, supplies
or merchandise are provided directly or indirectly to a Medi-Cal recipient.
A post office box or commercial box is not a business address.
PIA account requests are submitted electronically to the DHCS Vision Services Branch
for review via the PIA Optical On-Line System, https://optical.pia.ca.gov/pool/
Accounts are not transferable.
*Forms and applications are available through Provider Enrollment Division found
through the Medi-Cal website at www.medi-cal.ca.gov
or contact the Telephone Service Center at (800) 541-5555.
-
How do I update my address information on the PIA Optical website?
Log into the CalPIA Optical Online website at https://optical.pia.ca.gov/pool.
Select the “Maintain Profile” menu tab and select the account management option
of “Address Change”, update the address and press “Submit Request.”
You will be notified by e-mail if approved.
New address must match the current professional license, Medi-Cal and vision plan
provider records (see requirements for #2). Temporary status
may be granted subject to DHCS review and approval.
As a reminder, providers are responsible to notify Medi-Cal Provider Enrollment
of address changes.
-
When we entered the prescription for a patient, we get the following message: “parameter(s)
requested exceeded the range of what can be fabricated at PIA…” What do we do?
Since the order is unable to be made at PIA, it must be obtained through a private lab of
your choice by seeking prior authorization for the service and subsequent reimbursement.
If the patient is enrolled in Managed Care Vision Plan, please obtain authorization by the
plan directly, such as VSP.
If the patient has Fee-for-Service, “straight”, Medi-Cal, please submit an Electronic
Treatment Authorization Request (eTAR) to Medi-Cal Vision Services Branch.
Tips for submitting a Vision eTAR on the Medi-Cal website, www.medi-cal.ca.gov:
- Select/Click on the <Transactions tab>, next click on <e-TAR>;
- Then select <Medical Services> to access the eTAR menu;
- Click on ->> <Create a New TAR>;
- Enter provider information. Fields designated with an asterisk (*) are required;
- Enter patient information when requested;
- Next, under <Other Services>, please select a Vision Service Category,
(i.e., Vision – Other Eye Appliances)
- Enter required information, including service code(s) that require a TAR, ICD-10 code. Medical
justification for the service is entered in the Enter Misc. TAR information field/box;
- Click on TAR summary to review the eTAR before submission;
- Please select an Attachment Submission Option then click ;
- After the TAR is submitted, a TAR number will be generated;
- Please wait for DHCS review;
- If approved, obtain lenses through a private lab of your choice (not PIA) and bill Medi-Cal with
invoice and TAR Control Number, TCN (enter on claim form as “prior authorization number”).
For further assistance, see Tutorial, or contact the Medi-Cal telephone call center at (800) 541-5555.
-
The patient’s eyeglass order was rejected because of Other Health Coverage (OHC).
What does this mean?
The Medi-Cal eligibility system indicates that the patient has OHC with Vision Benefits.
The provider should contact that OHC plan for services since
Medi-Cal is not involved. If the patient denies having OHC, please
refer the patient to his/her county social services for resolution.
-
The patient’s eyeglass order was rejected because of remaining Share of Cost (SOC).
What does this mean?
Since this patient has remaining SOC/Spend down, he/she is not eligible for Medi-Cal/CalPIA
services. Beneficiary’s monthly SOC/Spend down dollar amount
must be cleared before he/she is qualified for Medi-Cal. Please
note if the SOC is used toward the patient’s eyeglass lenses, the order must go
to a private laboratory, not PIA, for fabrication.
-
What is the criteria for ordering polycarbonate lenses for patients 18 yrs. and
older?
Must have one of the following visual impairment in one or both eyes:
- best corrected visual acuity of 20/60 or worse
- restricted visual field of ten degrees or less
Please note polycarbonate lens orders must meet Medi-Cal minimum prescription requirements.
For example, plano protective lenses are not covered.
-
Who to contact regarding Medi-Cal billing questions?
For patients covered under managed care vision plans, please contact the plans (e.g.,
VSP) directly. For Medi-Cal Fee-For-Service (FFS), billing information
can be found in the Medi-Cal Vision Care Provider Manual available at
www.medi-cal.ca.gov or call the Telephone Service Center (TSC) at (800)
541-5555.
-
Are there limits to the number of eyeglasses covered?
Yes. Eyeglasses are covered once every 24 months.
There are limitations; state law says orders or replacements are subject to utilization
controls set by the Department of Health Care Services.
-
Who is eligible for CalPIA eyeglasses lens services?
Medi-Cal beneficiaries under 21 years of age with full benefits eligibility.
Exceptions to this are Medi-Cal beneficiaries 21 years of age and older receiving
long-term care in a skilled nursing facility or intermediate care facility and those
who are pregnant.
(Effective January 1, 2020, Medi-Cal adult optical benefits are restored to beneficiaries ages 21 and older).
-
Effective February 1st 2020, courier services will be provided by Unity Courier Services. Please call 1-800-992-8890 or visit
http://dst.unitycourier.com to schedule a pick-up.
Reminder: Please select courier labels to assigned CALPIA lab shown on printed orders. The counties of Orange, Stanislaus and San Joaquin
will now be serviced by CSP-Solano Optical laboratory.
-
How to place a REDO order with the lab?
Login in, select Order Status, enter the 7 character Rx number of the order requiring redo. By click-selecting the previous order, the Rx
information page appears.
To proceed with REDO, entering the reason (via the drop down menu) and type of REDO (select button) on bottom.
Next, the system will generate a new order with a new Rx # (begins with letter 'R' for LAB REDO, 'D' for DR. REDO). Review the order or
edit (only allowed for DR. REDOs). Submit.
Reminders: Don’t forget to click on Submit to execute the order into the system before printing Rx form and shipping. Please return the
lenses with your resubmission.
-
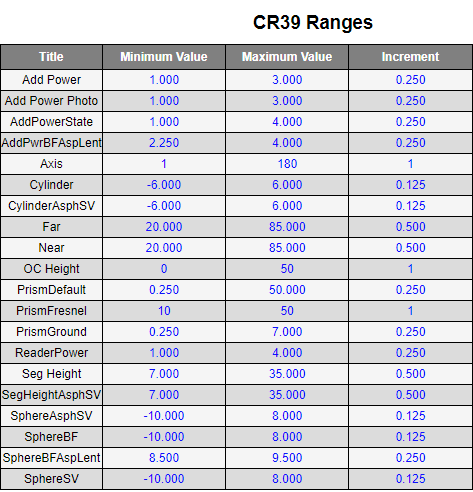
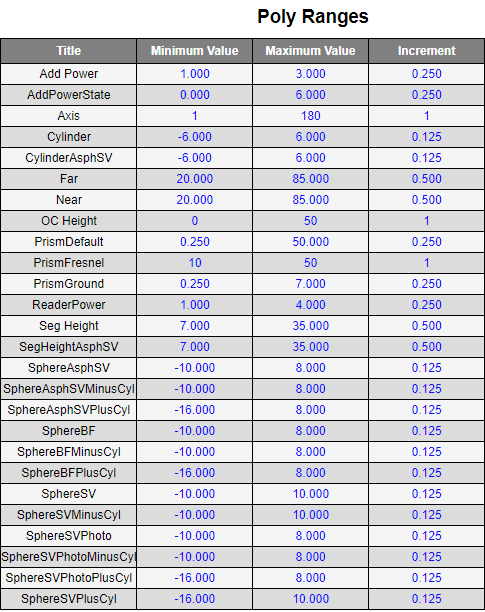
What are the accepted power ranges in diopters for the PIA labs for polycarbonate and standard plastic lenses?
CR39 Plastic Ranges
Polycarbonate Plastic Ranges
-
The California Prison Industry Authority (CALPIA) is not a patient point of contact regarding
access to, requesting copies, or requesting amendments to their health information records. All
inquiries shall be directed to the optometrist or optician that the patient ordered from.
It is the objective of CALPIA to protect patient privacy rights while ensuring timely and accurate
access to their health records. This can be accomplished by providing guidance to optometrists and
opticians authorized to enter optical orders through the PIA Optical On-Line System (POOLS).
CALPIA adheres to federal and state regulations concerning patient health information and patients’
rights to access, amend, and personal disclose their health information. This policy outlines the
rules and responsibilities for ensuring CALPIA maintains compliance with federal and state regulations,
including the Health Insurance Portability and Accountability Act (HIPAA) and relevant California laws.
Patients Right to Access Health Information
-
CALPIA is not a patient point of contact and will refer all inquiries to the authorized optometrist or optician that the patient ordered from.
-
CALPIA provides the following guidance to authorized optometrists and opticians to ensure they understand the following:
- Patients' rights to access their health information is clearly described.
- They shall respond to all patient requests for access to their health information.
- Patients have the right to obtain health information records from their optometrist or
optician in the format they choose.
- They shall notify the patient if additional time is needed to address the request.
- They must describe the denial of access and appeal process, including reasons for denial,
explanations to the patient, handling of appeals, designation of a licensed healthcare
professional to review denials/appeals, et cetera.
-
Upon receiving a patient request to access, inspect, or receive a copy of their health information, optometrists and opticians understand that they shall:
- Provide copies of health information within 30 days.
- Provide copies within 15 days following an inspection of records.
- Advise the patient in writing within 60 days where to direct their request if the
Optometrist or Optician does not maintain the designated record set.
- Ensure cost-based fees do not exceed ten (10) cents per page.
Patients Right to Amend Health Information
-
CALPIA does not process amendment requests directly and will refer all such inquiries to the
appropriate optometrist or optician.
-
CALPIA provides the following guidance to optometrists and opticians to ensure they understand:
- Patients have the right to request amendments to their health information from their
optometrist or optician, which must be done in writing.
- They must advise patients in advance of the requirement for written requests through
the Notice of Privacy Practices.
- They ensure that correspondence regarding amendment requests must be filed in the
patient’s medical record and accessible to optometrist and optician staff.
- They respond to initial amendment requests within 30 days by either amending the record
or denying the request.
- They respond to appeals of denial within 30 days or notify the patient of an additional
30-day extension.
- They may deny amendment requests if the information was not created by them, would not be
available for inspection, or is accurate and complete.
- They understand that denial notifications must be written in plain language and include
the reason for refusal, process for review by a designated official, patient’s right to
submit a disagreement statement, and how to file a complaint.
- Documentation related to amendment requests must be retained for six years, including
the patient’s request, denial communication, statement of disagreement, and written
rebuttal.
Patient’s Right to Disclose Health Information
-
CALPIA does not process disclosure authorization communications and will refer all such
patient inquiries to the appropriate optometrist or optician.
-
CALPIA provides the following guidance to optometrists and opticians to ensure they understand:
- Health information can be used or disclosed without authorization under specified circumstances; all other uses and disclosures require prior authorization from the patient.
- Authorizations must be written in plain language and displayed in 14-point font.
- Procedures for processing authorizations must include handling modifications, revocations, and defective authorizations.
- Authorizations and related documentation are retained for a minimum of six years.
-
Authorizations must include:
- A specific description of the health information to be disclosed.
- Identification of persons or organizations requesting the information.
- The purpose of the disclosure.
- Expiration date or event.
- Patient signature and date signed.
-
CALPIA staff, optometrists and opticians authorized to access POOLS shall review information
assets and records on an annual basis to ensure information use is in compliance with state and
federal law, regulation, and policy. Reviews shall include notices of collection and the privacy
policy and shall be updated to reflect current practices.
|